By: Amanda Oleiro
November 30, 2021

On the morning of Aug. 4, 2021, my 11-month-old son had his first seizure. None of us knew it was a seizure, but as the next 24 hours unfolded and brought on three more, we'd come to figure it out. Figuring out why, however, turned out to be a lot more complicated. And as a concerned parent, playing the diagnosis waiting game wasn't easy.
That being said, when I relive that day and the months that followed, I realize I learned quite a bit during that wait, starting with the No. 1 parent rule:
Trust your intuition.
Two hours after I dropped my son off at day care, I got a call saying he had spiked a 102 fever. I was a bit taken aback, seeing as he hadn't shown even the slightest hint of a sickness earlier that morning. But as parents quickly learn, kids are full of surprises, and I figured this was just one of those days.
In the five minutes it took me to drive to day care, my kid had become completely inconsolable and was crying a cry I had never heard before. They told me he had just vomited, and I thought to myself, "Huh, this must be his bellyache cry. Weird."
I got him home, and we spent the rest of the day napping, snuggling and snacking. We had just finished dinner, and as I turned to pull him out of his highchair, I realized his entire left cheek was twitching — as if someone were pulling an invisible string attached to his cheek over and over and over again. At first, I thought maybe my son discovered a new silly trick, but once my "Whatcha doin', silly?" turned into a "Hey, buddy, you OK?" with no reaction, I knew something was wrong.
I vaguely remembered our pediatrician saying something about repetitive movements when our kiddo was just a few weeks old — that if we saw any, they could potentially be a seizure. Seizure. It hit me. This was a seizure. My kid was having a seizure.
I immediately FaceTimed my husband, who was out of town on a work trip. I needed someone else to see what I was seeing and confirm it wasn't normal. He could hear the panic in my voice right away as I held our son up to the phone and said, "Look at him — I think something is wrong." My husband told me to take our son to the ER immediately.
By the time I got my shoes on, my son was completely unresponsive and turning blue. The twitch persisted. I panicked. Do I call 911 or drive myself? But before I could pick up my phone, the twitching stopped. He snapped out of it and started to cry — that very distinct cry I had never heard until just nine hours earlier.
I got him in the car and drove straight to the Children's ER — which, conveniently, was just 10 minutes away. They ran some tests and observed us for a few hours. Everything came back normal. The doctors explained to me that with his fever, it was likely he had a febrile seizure, which was totally normal for his age, and that the chances of him having another during the same sickness were extremely low. They sent us home.
Use your health care team to prepare for the "what ifs."
Despite me telling him everything was fine, my husband decided to make the three-hour drive home and arrived around 1 a.m. I'm glad he did, because just after 2 a.m., our son seized again. This time, it was a full-body, convulsive, eyes-rolled-back, arched-back kind of seizure.
We were both terrified, but seeing as I had already done this once before, I was able to compose myself enough to walk us through what I had just learned nine hours earlier at the ER.
Step 1: We have to clock it — anything over five minutes is considered an emergency "call 911" situation.
Step 2: We have to make sure his airway doesn't get blocked by his tongue, which in this moment meant I had to hold him at a slight angle.
Step 3: Wait — for up to five agonizing minutes, simply wait.
After about three minutes, the convulsions stopped. He snapped out of it. And he cried what I then knew was his seizure cry. I told my husband we were heading back to the ER. Even though the seizure was under five minutes and therefore not a "medical emergency," I was determined to find out what was going on.
They admitted us right away and ran a whole new slew of tests. As the hours passed, lab test after lab test came back clear. The doctors couldn't figure out what was causing my son's fevers, but they seemed under control. And although two febrile seizures with the same sickness is rare, it's possible with what's termed "complex febrile seizures." They decided to discharge us.
As we were waiting for paperwork, I felt my son start to get warm again. I asked the nurse if she could give us a dose of Tylenol for the road, and she agreed — it was time for a new dose anyway. Two minutes after we squeezed the cherry-flavored goo into his mouth, and nine hours after his last seizure, he seized again. Full body, convulsive, eyes rolled back, arched back — only this time, he was hooked up to the monitors. That meant, in addition to watching my son turn blue for a third time, I saw his oxygen levels plummet to the 40s as an entire team of doctors ran into the room and nurses pumped oxygen into his tiny lungs.
Three minutes later, it stopped. He came to. And he cried. And through my own tears, I told the doctor, "That's his seizure cry."
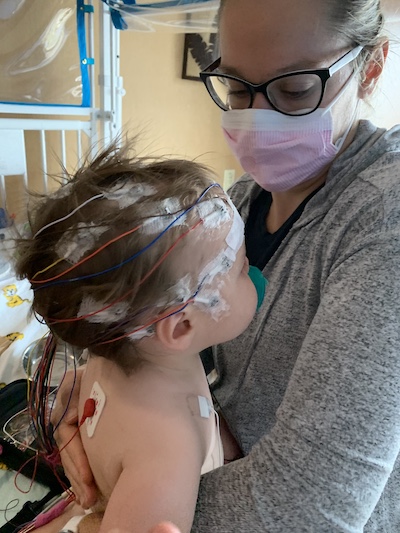
They scheduled an electroencephalogram (EEG) and MRI immediately. If you, like me three months ago, are not familiar with an EEG, the procedure consists of gluing 26 electrodes to a person's head so a neurologist can monitor their brain waves. For a normal, calm person, applying the electrodes takes about an hour. For a terrified and traumatized 1-year-old, the process takes a light sedative, three adults and two hours' worth of fighting.
And that's just to get the electrodes on. You then have to keep them on for hours, tethered to a machine while a camera watches your every move. Our son's EEG lasted about 15 hours — long enough for the neuro team to confirm our son was having clusters of seizure-like activity that were building up into full-blown seizures (which explained the nine-hour cycle we seemed to be working with). They started him on anti-seizure medication right away.
Then they sent him for an MRI to see if they could identify a cause for these abnormal brain waves. It came back clear. While he was sedated, they also did a lumbar puncture to retrieve spinal fluid for a culture to rule out meningitis. It too, came back clear. After a discussion with the neuro team and general pediatrics team, we headed home armed with seizure meds and follow-up appointments.
Find a balance of trusting the experts and doing your own research.
Our first follow-up was with our pediatrician, who happened to be doing rounds in the hospital the entire time our son was admitted. He knew everything and was eager to hear how things were a week later. Luckily, we had nothing abnormal to report. "Good," he told us. "Because epilepsy can cause delays and regressions, so you have to pay close attention to the milestones." I had no idea.
I asked our doctor, "So our son has epilepsy? Is that what we're officially saying?" He responded, "We're treating this as epilepsy." He explained to me that with how many seizures my son had — which ended up being four once we connected the dots to the day care episode (isolated to just his lips) — it put him in the territory of epilepsy or some other seizure disorder. The protocol was to treat it as such until we knew more.
He then handed me a massive packet of epilepsy information explaining triggers and safety and all sorts of things you never want to have to worry about for your kid. Once we were home, I whizzed through the packet, taking special note of the "seizure action plan" section, and went to multiple epilepsy websites to do a little research of my own.
Again, I had no idea how complex the condition was. I had no idea there were all sorts of classifications for seizures broken down by where it affects the brain (one spot or the entire brain), what the seizures look like (stiffness versus limp, jerking versus still) and whether the person is aware or not. I also had no idea there were hundreds of potential triggers — sicknesses, lack of sleep, certain times of the day, growth spurts, hormonal changes, low blood sugar and on and on and on. There is even a bath-related epilepsy!
As helpful as the medical sites were, for my own understanding, I realized I also needed personal insights from other parents. I decided to join an epilepsy Facebook group, which gave me a constant feed of firsthand experiences that drastically expanded my awareness and knowledge of the condition. The combination — our medical team, the background knowledge and personal stories — made me feel as though I was going into "the unknown" as prepared as possible.
Accept the waiting game…
We met with the pediatric neurologist (who works closely with our pediatrician) and created a plan to move forward. Part of the plan was to figure out medications. The doctor explained our son was on the "catch-all, go-to medication" to prevent seizures and that it was an effective medication but known to cause major mood swings and sleep issues. Our son was experiencing both, but since he had only been on it for a couple weeks, we decided to wait a little longer to see if he'd settle into it. Waiting, we quickly realized, is a big part of treating seizure disorders.
The second part of our plan was to do an epilepsy genetic test (which tests over 290 epilepsy-related genes) to see if anything popped up that could guide the medications or give us a hint as to whether we were dealing with an epilepsy my son could grow out of. After four weeks, we got the results. Fortunately and unfortunately, it didn't have any significant finds to help pinpoint our diagnosis.
But know when to stop waiting.
Our kid's moods weren't improving and paired with the hours of restlessness he had each night, things were beginning to feel unsustainable. So, as moms tend to do, I scoured the internet for potential hints and answers for my son's condition. I learned from the Facebook group that there are multiple medications, each with their own strengths and weakness. And it was super common to have to add meds, switch meds, wean from meds, etc.
After a quick message to our doctor, he switched the med. To our surprise, our son's moods improved, and he didn't have any breakthrough seizures. His sleep was still an issue, but hey, in the words of Meatloaf, two out of three ain't bad. All things considered, we felt lucky, but still wanted answers.
Advocate for your kid.
Night after night, my son's sleep continued to suffer. We also noticed he started having staring spells here and there, which per my internet research findings could be completely normal for a daydreaming 1-year-old, or they could be seizures. I messaged the doctor again.
He told us we could add a medication to hopefully help with the restlessness. But with the staring spells and not really knowing what was happening with our kid outside of my own observations, I requested another EEG, just to be sure.
Our doctor had already planned to do a repeat EEG six months after our son's first EEG, but given the fact that we had switched meds and were potentially seeing some breakthrough activity, our doctor agreed to bump it up a few months. We endured another round of gluing 26 electrodes to my son's head — though thanks to "Cocomelon," this round was much smoother than the first — and waited 24 hours inside our hospital room for the results.
The next morning, a doctor from the neuro team came into our room and gave us the news: Our son's EEG was completely normal. No seizure activity. The night stirs were likely a result of the medication throwing off his sleep cycles (not nocturnal epilepsy). And although we didn't catch any staring spells on the EEG, that wasn't as much of a concern given the great results.
His verdict: My son doesn't have epilepsy.
My husband and I looked at each other, first shocked. Then relieved. Then confused. We looked back at the doctor, and I hesitantly asked, not wanting to give up the glimmer of hope and relief I was starting to let myself feel for the first time in months:
"Then what caused his seizures in the first place?"
His response: Likely a virus.
It's still unknown as to which. But thanks to our neuro doc walking us through multiple moments before and after the seizures, we were able to put enough of the pieces together to narrow it down.
We're not officially in the clear. This sort of diagnosis is complex and waiting comes with the territory. The plan is to keep my son on medication a little longer so we can hopefully hit the six-month seizure-free milestone. We're told once you hit six months, your chances of having another seizure drop drastically. After that, we'll wean off the meds, and … wait.
We're not in the clear, but for the first time in our diagnosis waiting game, we're extremely hopeful.
*Amanda is an employee of MU Health Care


